Overview
Overview
A COMPARATIVE EFFECTIVENESS STUDY ON CATHETER LOCKING DEVICE VERSUS STANDARD VENTRICULOSTOMY FOR SURGICAL MANAGEMENT OF TRAUMATIC BRAIN INJURY PATIENTS WITH INTRACRANIAL COMPARTMENT SYNDROME.
Patients who have suffered traumatic brain injury (TBI) often require urgent surgical interventions to control intracranial pressure (ICP). Elevated ICP poses life-threatening risks by compromising cerebral perfusion and causing severe neurological damage. Intracranial hypertension is a common complication in severe TBI cases, often caused by factors such as intracranial hemorrhage, cerebrospinal fluid (CSF) accumulation, or cerebral edema, which creates a mass effect that increases pressure within the cranial vault. This mass effect reduces
blood flow and oxygen supply to the brain, heightening the risk of irreversible neuronal damage (1).
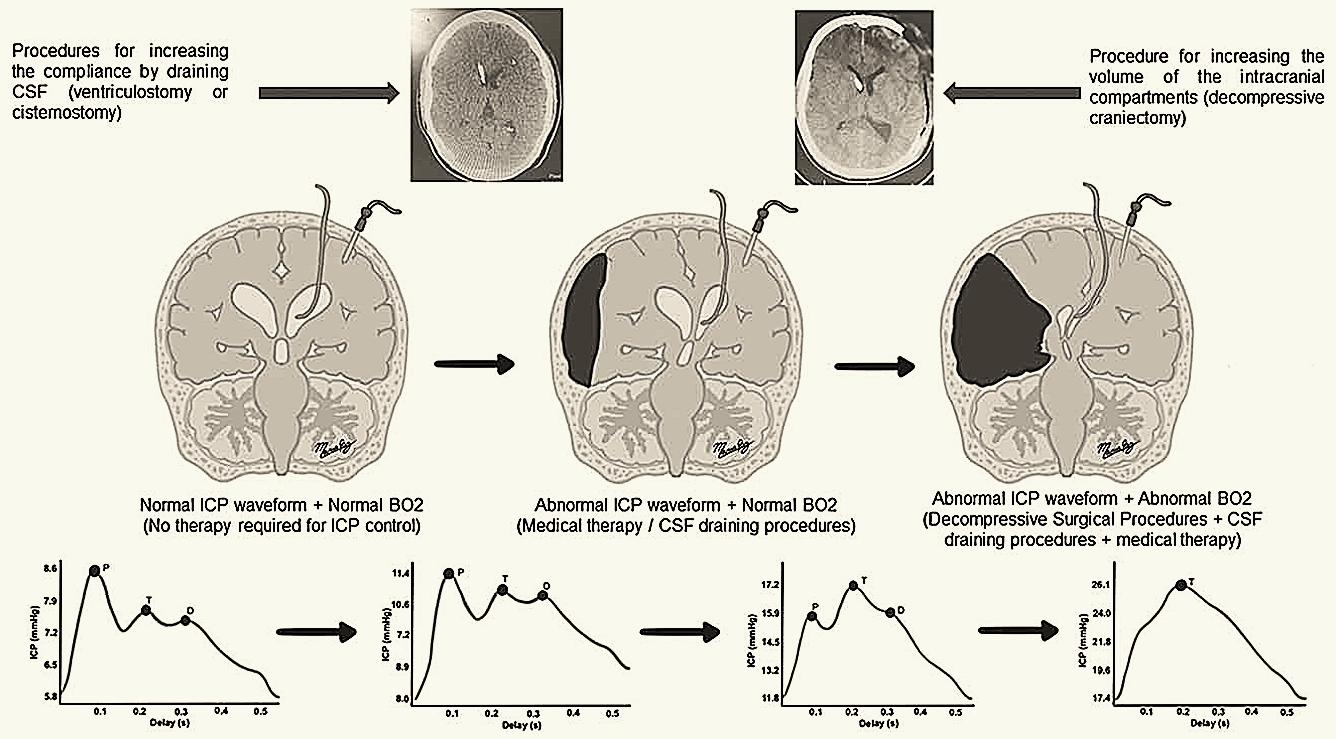
In cases of increased ICP, the primary goal of neurosurgical intervention is to reduce this pressure to preserve brain tissue integrity and prevent neuronal injury. Several procedures can achieve this goal, each targeting different intracranial compartments to expand cranial vault capacity and facilitate brain expansion. These procedures are essential when physiological compensatory mechanisms (such as CSF redistribution and reduced cerebral blood volume) are overwhelmed.
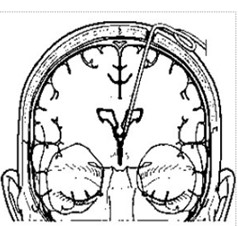
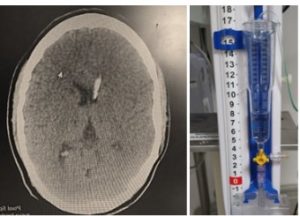
Among therapeutic options, ventriculostomy or external ventricular drainage (EVD) is a preferred technique for managing intracranial hypertension. Ventriculostomy involves the insertion of a catheter into the brain’s ventricular system to drain CSF in a controlled manner, directly reducing ICP. This procedure is performed by opening a burr hole in the skull through which the catheter is guided into the lateral ventricles, allowing the drainage of accumulated CSF that exerts pressure on intracranial structures. This intervention is particularly useful in conditions like hydrocephalus, where pathological CSF accumulation in the brain’s ventricles dangerously elevates ICP, thereby compromising the patient’s neurological function (2-3).
In addition to its therapeutic role, ventriculostomy offers the added advantage of allowing real- time ICP monitoring. This monitoring capability is crucial, as it provides live data on intracranial pressure, enabling the clinical team to adjust and optimize treatment according to the patient’s
immediate needs, thus improving success rates and reducing potential complications. Although ventriculostomy is generally considered a second-line therapy, it can be highly effective in cases where CSF drainage provides a rapid and precise reduction in ICP. This lessens the impact of the intracranial compartment syndrome (ICCS) and improves the patient’s prognosis (4).
Recent clinical studies and consensus guidelines from anesthesiology and neurocritical care societies on ventriculostomy management highlight spontaneous catheter displacement as one of the most common complications. This issue is significant due to its impact on the effectiveness of ventricular drainage and the potential need for surgical revision. These studies emphasize the importance of precise surgical techniques and auxiliary devices to minimize ventriculostomy complications, particularly catheter displacement (5, 6).
The objective of this study is to determine the outcomes of standard ventriculostomy versus the use of a locking system for the ventricular catheter in the surgical management of patients with TBI and intracranial compartment syndrome.
- Hawryluk GWJ, Citerio G, Hutchinson P, Kolias A, Meyfroidt G, Robba C, Stocchetti N, Chesnut R. Intracranial pressure: current perspectives on
physiology and monitoring. Intensive Care Med. 2022 Oct;48(10):1471-1481. doi: 10.1007/s00134-022-06786-y. - Chau CYC, Craven CL, Rubiano AM, Adams H, Tülü S, Czosnyka M, Servadei F, Ercole A, Hutchinson PJ, Kolias AG. The Evolution of the Role of External Ventricular Drainage in Traumatic Brain Injury. J. Clin. Med. 2019, 8, 1422.
- Srinivasan VM, O'Neill BR, Jho D, Whiting DM, Oh MY. The history of external ventricular drainage. J Neurosurg. 2014 Jan;120(1):228-36. doi: 10.3171/2013.6.JNS121577.
- Rubiano AM, Figaji A, Hawryluk GW. Intracranial pressure management: moving beyond guidelines. Curr Opin Crit Care. 2022 Apr 1;28(2):101-110. doi: 10.1097/MCC.0000000000000920.
- Dakson A, Kameda-Smith M, Staudt MD, Lavergne P, Makarenko S, Eagles ME, Ghayur H, Guo RC, Althagafi A, Chainey J, Touchette CJ, Elliott C, Iorio-Morin C, Tso MK, Greene R, Bargone L, Christie SD. A nationwide prospective multicenter study of external ventricular drainage: accuracy, safety, and related complications. J Neurosurg. 2021 Nov 26;137(1):249-257. doi: 10.3171/2021.7.JNS21421.
- Lele AV, Hoefnagel AL, Schloemerkemper N, Wyler DA, Chaikittisilpa N, Vavilala MS, Naik BI, Williams JH, Venkat Raghavan L, Koerner IP; Representing SNACC Task Force for Developing Guidelines for Perioperative Management of External Ventricular and Lumbar Drains. Perioperative Management of Adult Patients with External Ventricular and Lumbar Drains: Guidelines From the Society for Neuroscience in Anesthesiology and Critical Care. J Neurosurg Anesthesiol. 2017 Jul;29(3):191-210. doi: 10.1097/ANA.0000000000000407.
Intracranial Compartment Syndrome
Intracranial Compartment Syndrome
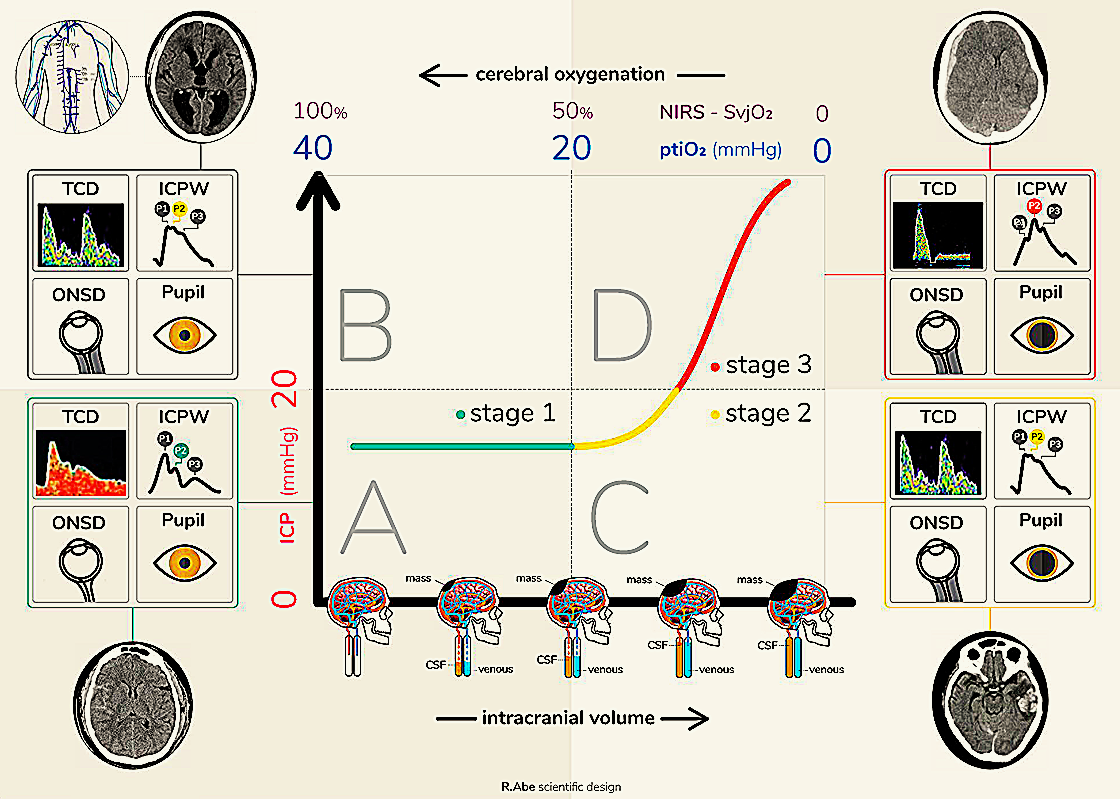
Intracranial compartment syndrome (ICCS) is a diagnostic model that identifies the loss of compliance in one or various cranial compartments. This corresponds to the point at which the compensatory mechanisms of intracranial pressure have been exhausted, leading to a compromised blood supply to the brain with subsequent ischemic cerebral injury.
The implementation of this model optimizes decision making for the treatment of patients with acute brain injuries since it allows the state of the intracranial compensatory reserve to be identified in a more integrated manner and to take into account individual variations that each patient may present that could modify the intracranial pressure threshold that is tolerated without injury to the brain tissue.
Analogous to how the management of intracranial hypertension is proposed, the treatment of ICCS has a tiered character, with cranial decompression surgical procedures considered as third-line measures to deal with the loss of cerebral compliance and prevent further brain ischemia.
Suggested readings:
- Rubiano, A. M., Figaji, A., & Hawryluk, G. W. (2022). Intracranial pressure management: moving beyond guidelines. Current opinion in critical care, 28(2), 101–110. https://doi.org/10.1097/MCC.0000000000000920
- Godoy, D. A., Brasil, S., Iaccarino, C., Paiva, W., & Rubiano, A. M. (2023). The intracranial compartmental syndrome: a proposed model for acute brain injury monitoring and management. Critical care (London, England), 27(1), 137. https://doi.org/10.1186/s13054-023-04427-4
- Godoy, D. A., Brasil, S., & Rubiano, A. M. (2024). Further support for the intracranial compartmental syndrome concept. Critical care (London, England), 28(1), 311. https://doi.org/10.1186/s13054-024-04974-4
Characteristics of the Study
Characteristics of the Study
This study will be a prospective, multicentric, observational, comparative-effectiveness enrolling patients from high developing index (HDI) regions and collecting also data in a group of countries from low and middle developing index (LMDI) regions. The data collection in these two different contexts will allow an understanding of the procedure´s impact on the outcome of patients from less-resourced areas. This second group of countries will be identified as areas of “humanitarian research”.
The study will include patients with TBI and ICCS managed either by standard ventriculostomy or ventriculostomy plus a locking system device. Patients with pre-existing neurological disorders will be excluded. In an instrumental analysis, outcomes between centers according to treatment preference will be compared, measured by the case-mix adjusted proportion per center. The primary outcome will be a functional outcome rated by the Glasgow Outcome Scale Extended at discharge and 3 months, 6 months, and 12 months after surgery, with specific ventriculostomy complication rates including infections, catheters coming out, and reinterventions. Statistical analysis will include ordinal regression as a common odds ratio (OR), adjusted for prespecified confounders. Variations between center preferences will be quantified with the median OR.
Demographic characteristics including vital signs, biochemical data, preoperative parameters at presentation, and intraoperative and postoperative variables will be collected from the study registry, including prehospital care, emergency care, surgical care, and intensive care data sections. The interviews for outcome evaluation will be performed on-site or by phone. Secondary outcomes will include aspects like control of the ICCS, frequency, and type of neurosurgical interventions, medical and surgical treatment intensity, surgical site complications, ICU, and in-hospital length of stay, including dichotomized GOSE score across multiple thresholds.

Locking Systems in Ventriculostomy
Locking Systems in Ventriculostomy
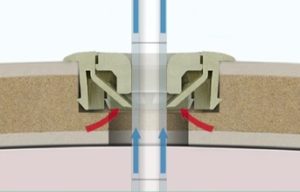
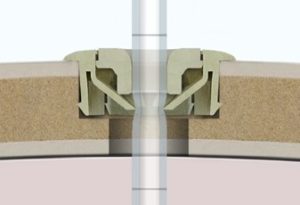
Assessment of locking systems in ventriculostomy for TBI involves evaluating their ability to ensure accurate, reliable, and safe CSF drainage. Proper locking systems minimize the risk of catheter displacement, prevent over-drainage, and maintain intracranial pressure control. These systems are essential in managing traumatic brain injury by reducing complications associated with elevated intracranial pressure. However, further studies are required to establish the optimal design, functionality, and clinical outcomes of various locking mechanisms. The adoption of advanced, evidence-based locking systems could enhance the safety and efficacy of ventriculostomy in this critical patient population.

Registry
- ClinicalTrials.gov ID: NCT06772155
- Registry site: https://clinicaltrials.
gov/study/NCT06772155?term= NCT06772155&rank=1
- ISRCTN ID: ISRCTN18208768
- Registry site: https://www.isrctn.com/
ISRCTN18208768?q= ISRCTN18208768.&filters=&sort= &offset=1&totalResults=1&page= 1&pageSize=10

